In medicine, a diagnosis is not always straightforward. Many diseases or conditions can present in various ways, depending on the circumstances. So how do you train for the uncommon presentations?
Case in Point allows radiologists to evaluate common findings as well as diseases and conditions that can present in interesting ways. The 2023 Case in Point Case of the Year, “superior mesenteric artery syndrome," is an example of the latter.
 |
 |
 |
Check out the case and then read on to learn more about the Case of the Year and its authors in this Q&A.
Why did you select this case for submission?
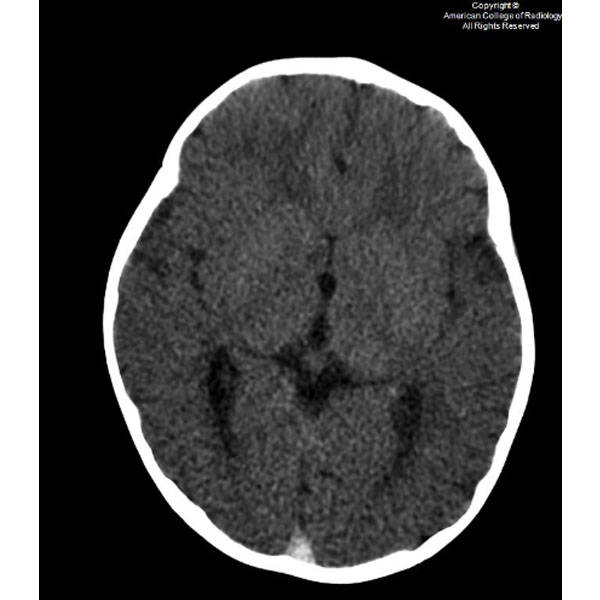
We selected this case because of its unique presentation and associated findings. The patient’s medical managing team was surprised when we communicated to them the finding of suspected gastric outlet obstruction on abdominal radiograph and recommended placement of an enteric tube with order for immediate cross-sectional imaging. They told us that the working diagnosis was constipation and were planning to treat it conservatively with enema. Follow-up computed tomography (CT) confirmed the upper gastrointestinal (GI) obstruction and revealed the underlying cause to be superior mesenteric artery (SMA) syndrome. The team was then able to elicit a history of significant rapid weight loss from the mother.
What should readers learn from this case?
Reading plain radiographs is an art that needs to be mastered by all radiologists. New trainees should be aware of the subtle, but information-laden clues to diagnosis that can show up on plain films and direct next steps of management.
What did you learn from working on the case?
We learned that prior cases have been published on the accepted normal aortomesenteric angle and distance along with the range of these values that are diagnostic for SMA syndrome. Also, coexistence of SMA and nutcracker syndrome is rare even though they share similar pathophysiology.
How did guidance from senior staff at your institution impact your learning and case development?
We were excited when our Attending, Dr. Hammill, agreed with our diagnosis. However, we were confused with the liver and splenic ischemic foci apparent on CT as this is not a phenomenon ever described to be associated with SMA syndrome. Dr. Hammill directed our attention to the compression of the retroperitoneal vascular structures including branches of the celiac artery by the markedly distended stomach.
Why did you choose Case in Point for submission of your case?
Case in Point is a valuable resource that enriches our residency education because we know we will not be directly exposed to every diagnosis during training. When we can review a variety of cases shared by others on the Case in Point platform, we are more confident that we will recognize them when they come up in the future.
Are you a regular reader of Case in Point? What are your favorite types of cases?
Yes. We especially appreciate cases that challenge us to identify and click on the abnormality. They help train the eyes to pick out abnormalities and the mind to identify patterns. The annotations on images also help to pinpoint exactly what is being described in the text.
What else should we know about the case that you’d like to share?
It was thrilling to see on follow-up imaging that the ischemic foci on the liver and spleen resolved after gastric decompression. It was also comforting that the patient could achieve relief with conservative management of refeeding and weight gain.
 |
 |
|||
| Hadassah Stein, MD PGY-1 Intern Year, Radiology Resident, Mather Hospital at Northwell Port Jefferson, NY |
Temitope Soyemi, MBBS PGY-5, Radiology Resident SUNY Downstate Brooklyn, NY |
 |
|||||||
| Patrick Hammill, MD Diagnostic Radiologist Kings County Hospital Center Brooklyn, NY |
|||||||
 |
 |
|
|
|
Congratulations to all case contributors.
The College could not maintain such a high level of quality without a steady supply of incredible cases.
Thank you to our Case in Point Associate Editor, Paul Hill, MD, for editing this case.